 |
Close
window to return
|
Issue 11, May 2001
The contribution of job insecurity to socio-economic
inequalities
Michael Marmot, Jane Ferrie, Katherine Newman and Stephen Stansfeld
- Over the past twenty years, socio-economic inequalities in mortality have widened. At the same time, patterns of employment, job security and welfare provision since the Second World War have undergone and continue to undergo major change. Future employment, for many people, is less certain.
- Job insecurity has started to attract research interest over the past decade. Studies of job insecurity attributed to workplace closure and self-reported job insecurity have demonstrated adverse effects on self-reported physical and mental health. However, well-designed, longitudinal studies remain rare and the contribution of job insecurity to inequalities in health uninvestigated.
- In this project, data from an ongoing, longitudinal study of civil servants and ex-civil servants were supplemented by new data collected by in-depth interview. These data have been used to examine the effects of self-perceived job insecurity over time, assess its contribution to inequalities in health, and explore the job insecurity-health relationship.
- Environmental factors, type of work, situational and individual characteristics emerged from the in-depth interviews as determinants of job insecurity. In addition to the threat of job loss, feelings of insecurity were generated by loss of valued features of the job and unwanted additional tasks and responsibilities. Factors which contributed to the job-insecurity-health relationship fell into five categories; personality and attitude, life events, work characteristics, other potentiating or ameliorating factors, and coping mechanisms.
- The explanatory potential of factors identified by interview were tested in data from all participants in employment. Pessimism, heightened vigilance, difficulty in paying bills, financial security, social support and job satisfaction explained much of the association between job insecurity and self-assessed health. With the addition of job control, the same factors explained most of the association with minor psychiatric morbidity and depression.
- An exploration of the effects of perceived job insecurity over time showed that, relative to workers who remained in secure employment, self-reported morbidity was raised among workers who lost job security. Workers exposed to chronic job insecurity had the highest self-reported morbidity, indicating that job insecurity acts as a chronic stressor. Among those who regained job security, adverse effects, particularly in the psychological sphere, were not completely reversed by removal of the threat.
- In our study population there have been slight increases in socio-economic differences in morbidity and cardiovascular risk factors over 11 years follow-up from the late 1980s. There has also been a significant widening of the gap for measures of minor psychiatric morbidity in both sexes and cholesterol in men. However, despite steep gradients in perceived job insecurity, with the exception of depression, adjustment for job insecurity had little effect on inequalities in morbidity and cardiovascular risk factors. Financial insecurity, on the other hand, contributed considerably to health inequalities, particularly in non-employed participants and men in paid employment.
- Current debate on the flexible labour market concentrates on direct economic returns. However, any deterioration in health has economic and social costs, which end up being borne by society. Policy makers should include these considerations in cost-benefit analyses of structural changes in the labour market.
Background
It has long
been accepted that occupation-related physical and chemical hazards contribute
to socio-economic gradients in mortality and ill health. Over the past
two decades the contributions of psycho-social characteristics of the
work environment, most notably job control and effort-reward imbalance,
have also increasingly been recognised. More recently, huge changes in
the nature of the labour market have brought another psycho-social work
characteristic, job insecurity, to attention.
Studies of job insecurity can be divided into those in which the exposure is self-reported and those in which it is externally attributed to downsizing or workplace closure. There is consistent evidence that self-perceived and attributed job insecurity have significant adverse effects on psychological morbidity and increasing evidence of adverse effects on self-reported physical health, but evidence of effects on physiological measures is weak and inconsistent (Ferrie 2001). Some work has documented associations between perceived job insecurity and personality characteristics or organisational measures, such as work effort. However, little attention has been paid to these or other factors as potential explanations of the job insecurity-health relationship.
Few studies have examined
job insecurity and socio-economic position. Therefore, there appears to
have been no work on the contribution of job insecurity to social gradients
in health. Similarly, longitudinal studies of perceived job insecurity
are still rare, and so the health effects of prolonged exposure remain
largely uninvestigated. Although transitions between job loss or unemployment
and re-employment in an insecure job have been examined (Ferrie et al,
200la), no studies have specifically investigated the effects of loss
or gain of perceived job security over time.
Aims
This project
addressed these gaps in understanding through Whitehall II, a longitudinal
study of civil servants and ex-civil servants in which steep employment
grade gradients in morbidity and cardiovascular risk factors have been
demonstrated. Restructuring of the Civil Service during the 1990s resulted
in large staff reductions, which disproportionately affected the lower
grades. Data on perceived job insecurity, collected during recent phases
of Whitehall II, enabled us to determine the contribution of job insecurity
to changes in inequalities in health, and examine the effects of change
in security and chronic insecurity over time. New data collection by in-depth
interview sought explanations of the job insecurity-health relationship
and a wealth of measures collected during the most recent phase of Whitehall
II enabled emerging associations to be tested in a wider population.
Data and Methods
Whitehall
II is an ongoing, longitudinal study of over 10,000 women and men, all
of whom were white-collar civil servants, aged between 35 and 55, when
the study started in 1985. Since the baseline data collection, which involved
a clinical screening and a questionnaire, there have been four further
data collection phases at regular intervals. Alternate phases collect
data by questionnaire only. In addition to analysis of quantitative data
from the Whitehall II study, we collected new qualitative data by in-depth
interview from a sub-sample of participants who perceived their job to
be insecure.
We used measures of job insecurity, financial insecurity, socio-economic circumstances, self-reported morbidity (covering general health, minor psychiatric morbidity, and longstanding illness), alcohol consumption and cigarette smoking from the questionnaire. Physiological measures (blood pressure, cholesterol and body mass index) were measured at clinical screening.
Other measures derived from the questionnaire were investigated as potential determinants or explanations of the job insecurity-health relationship. Aspects of personality and attitude: optimism- pessimism, emotional action and heightened vigilance; material measures: difficulty paying bills, personal income, household income, and wealth; other psycho-social work characteristics: job control, job demands and work social support.
Results
During the
most recent data collection for the Whitehall II study (1997-99), just
under half (46%) of the participants were still working in the Civil Service.
The majority who had left were not working (35%), but a sizeable minority
were employed elsewhere (19%). Thirty percent of women and 25% of men
reported job insecurity, which displayed steep employment grade and social
class gradients.
Processes through
which perceived job insecurity is related to health and other outcomes
Interviewees
discussed at length several sets of factors, which preceded the onset
of job insecurity: environmental factors, type of work, situational and
individual characteristics. Principal environmental factors were government
policy and the general climate of uncertainty generated by other redundancies
and public discourse on flexibility. Those who felt their work had been
rendered redundant, or was suitable for outsourcing, described an underlying
threat, which surfaced whenever the work came under scrutiny. Long tenure
and diminishing opportunities contributed to feelings of job insecurity
within the Civil Service, while previous experience of unemployment enhanced
vulnerability outside. Most participants were in their early to mid-50s
and job insecurity had pushed them unwillingly to consider whether to
retire early or try for another job. Single women dominated the group
most adversely affected by job insecurity or loss.
Job insecurity was not only generated by potential job loss. Interviewees also described feelings of increased vulnerability when valued features of the job were threatened or removed. Similar feelings were engendered on being assigned unwanted additional tasks and responsibilities, including private sector practices, previously alien to civil servants.
Potential explanations of the job insecurity-health relationship fell into five categories: personality and attitude, life events, work characteristics, other potentiating or ameliorating factors, and coping mechanisms. When describing their vulnerability to job insecurity, interviewees articulated certain personality characteristics including: directly low self-esteem, cautiousness, and aversion to change. Others, such as heightened vigilance, were evident from the interviews. Interviewees found it most difficult to cope when job insecurity coincided with other life events like bereavement.
Decreasing job satisfaction and control, and increasing demands, which included heavier workloads, tighter deadlines, longer hours and work taken home, emerged as the strongest potential mediators of the effects of job insecurity. Other factors that affected severity of the job threat were psychological dependence, perceived ease of obtaining alternative employment, support outside work, and financial security. Participants coped with job insecurity or loss in ways which were problem-focused, (such as networking), or emotion-focused, (such as adoption of the sick role) - and often both.
In addition to effects on health, predominantly discussed in terms of stress, perceived job insecurity had adverse effects on attitudes to work, and quality and quantity of home-life.
Perceived job insecurity
and health: potential explanations of the relationship
Potential
explanations of the job insecurity-health relationship identified through
the qualitative analyses were tested using data from all participants
in employment. Health outcomes in workers reporting job insecurity were
compared with outcomes for the securely employed, adjusted for pre-existing
ill-health at baseline, a period of secure employment for all participants.
Poor self-assessed health and measures of minor psychiatric morbidity were significantly higher among insecure workers of both sexes, but cholesterol in both sexes and body mass index in women were lower. Pessimism, heightened vigilance, difficulty in paying bills, financial security, social support and job satisfaction explained 68% of the association between job insecurity and self-assessed health in women and 36% in men (see Figure 1). With the addition of job control, the same factors explained 60% of the association with minor psychiatric morbidity and over 80% of the association with depression.
Chronic job insecurity
and change in job security
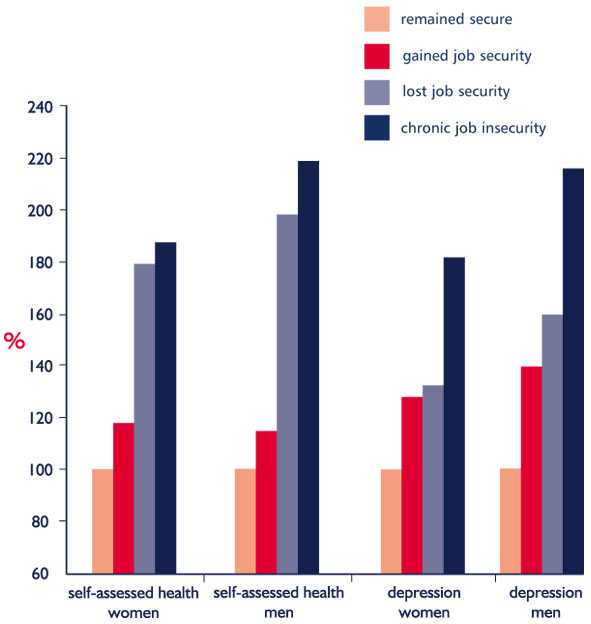
Figure 2
shows the health effects of loss or gain of job security between the two
most recent phases of the Whitehall n study (2½ years), and of
job insecurity at both phases, by comparing morbidity and cardiovascular
risk factors with outcomes for participants who had remained secure. All
analyses were adjusted for baseline ill health.
Among workers who gained security, residual negative effects of prior job insecurity were observed, particularly in the psychological sphere. There was greater self-reported morbidity among workers who lost job security between the phases, but those reporting chronic job insecurity had the highest levels (see Figure 2). Cholesterol decreased slightly in all workers who became or remained insecure. In women, loss of security was associated with higher blood pressure and chronic job insecurity with lower body mass index (Ferrie et al 200lb).
Change in health
inequalities
Steep employment
grade gradients in morbidity and cardiovascular risk factors were demonstrated
in the Whitehall II cohort at baseline and again during the most recent
data collection (1997-99). Comparison of 1997-99 gradients with those
at baseline showed a slight widening for most measures over the 11 years
follow-up. For minor psychiatric morbidity in both sexes and cholesterol
in men, this widening was significant (Ferrie et al 2001c).
Job insecurity
and financial insecurity: contributions to inequalities in health
Gradients
in morbidity and cardiovascular risk factors were slightly steeper in
non-employed participants than among those in paid employment. Despite
steep gradients in job insecurity among the employed, with the exception
of depression, adjustment for job insecurity had little effect on these
gradients. Steep gradients in financial insecurity, observed in employed
and non-employed participants, contributed considerably to gradients in
morbidity and risk factors, particularly for non-employed participants
and men in paid employment (Ferrie et al 200ld).
Conclusions and
Policy Implications
Using a
longitudinal design and adjusting for pre-existing ill-health, this study
has produced robust evidence that perceived job insecurity is associated
with increased morbidity, in particular mental ill-health. Pessimism,
heightened vigilance, difficulty in paying bills, financial insecurity,
lack of social support, job dissatisfaction and low job control explain
a considerable proportion of this association.
We have documented the tendency for socio-economic differences in morbidity and cardiovascular risk factors to widen over the 11 years from the late 1980s. Steep employment grade gradients in perceived job insecurity contributed little to these gradients, but financial insecurity contributed considerably to gradients in non-employed women and men and men in paid employment. These findings point to the need for policies which ensure adequate financial provision for the unemployed and those who 'volunteer' to leave the workforce early in the face of retrenchment.
Loss of perceived job security has adverse effects on self-reported morbidity, which is not entirely reversed by regaining security. Workers reporting repeated exposure to job insecurity have the poorest self-reported health, indicating that job insecurity acts as a chronic stressor. Policies whose direct consequence is to increase job insecurity should take into account the finding that periods of insecurity have residual effects, which are not reversed by removal of the threat. When impossible to avoid, any period of job insecurity should be resolved as soon as possible to avoid the health consequences of exposing workers to a chronic stressor.
There is current debate on the benefits of the flexible labour market to the national economy. To this consideration must be added the costs of damage to the individual and society, which in addition to personal misery, have economic consequences of their own.
This project was funded
under the ESRC Health Variations programme and was based in the Department
of Epidemiology and Public Health at University College London. The project
ran from December 1998 to November 2000.
Figure 1: Association of job-insecurity to health and effect of adjustment
for potential explanatory factors
The left-hand bar
in each histogram shows the measure of morbidity adjusted for age, employment
grade and baseline ill health. This represents the unexplained association
between job insecurity and health.
The right-hand bar of each histogram shows the measure of morbidity additionally
adjusted for all potential explanatory factors.
(1) pessimism, vigilance, difficulty in paying bills, financial security,
social support and job satisfaction
(2 )pessimism, vigilance, difficulty in paying bills, financial security,
social support, job satisfaction and job control.
Figure
2: Effects of loss or gain of job security and chronic job insecurity
on self-assessed health and minor psychiatric morbidity over 2.5 years
Selected papers drawn on for these Findings
Ferrie, J. E. (2001)
'Is job insecurity harmful to health?' Journal of the Royal Society
of Medicine 2001 94 : 71-76.
Ferrie, J. E., Martikainen, P., Shipley, M. S., Marmot, M. G., Stansfeld,
S. and Davey Smith, G. (2001a) 'Employment status and health after privatisation
in white collar civil servants: prospective cohort study.' British
Medical Journal 322 : 647-51.
Ferrie, J. E., Newman, K., Stansfeld, S. A. and Marmot, M. (forthcoming)
'The confounding of job insecurity in white-collar workers.'
Ferrie, J. E., Shipley, M. J., Stansfeld, S. A. and Marmot, M. (submitted)
'Effects of chronic perceived job insecurity and change in job security
on morbidity and cardiovascular risk factors in British civil servants:
the Whitehall II study'. 200lb.
Ferrie, J. E., Shipley, M. J., Davey Smith, G., Stansfeld, S. A. and Marmot,
M. (submitted) 'Change in health inequalities among British civil servants:
the Whitehall II study'. 200lc.
Ferrie, J. E., Shipley, M. J., Stansfeld, S. A., Davey Smith, G. and Marmot,
M. (submitted) 'Future uncertainty and socio-economic inequalities in
health: the Whitehall II study'. 200ld.
Contact:
Dr Jane Ferrie
Department of Epidemiology and Public Health
University College London
1- 19 Torrington Place
London
WC1E 6BT