According to a study by Ahmed et. al (2015) it is anticipated that 1 in 2 people in the UK will get cancer at some point in their lives. This is due to a number of factors but it is mostly because cancer is more common in the elderly, and due to advances in medicine and healthcare, there is a growing elderly population.
There are things that can be done to make getting cancer less likely (not smoking, reducing alcohol intake, eating healthy) but if you get cancer what can be done to treat it?
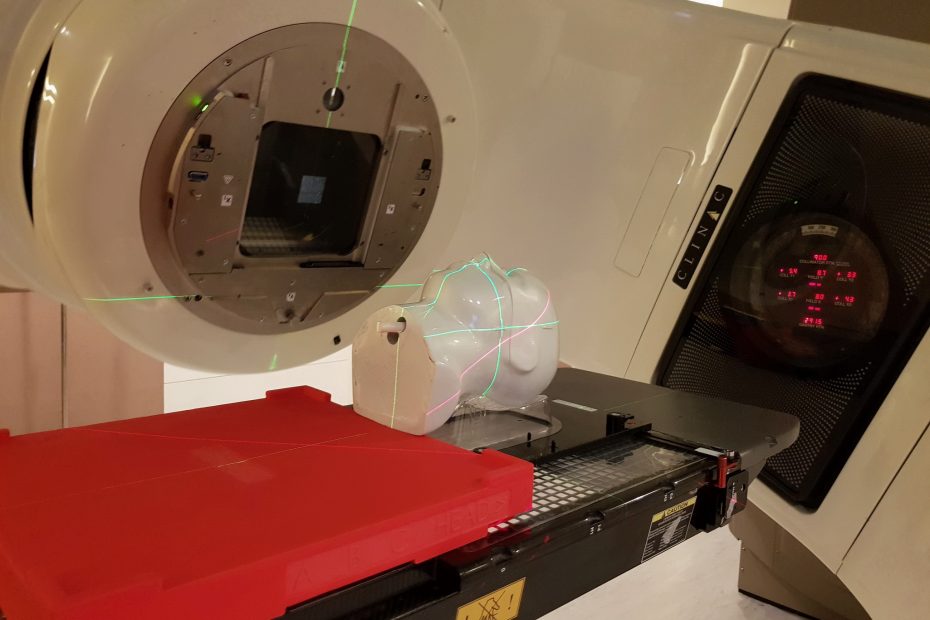
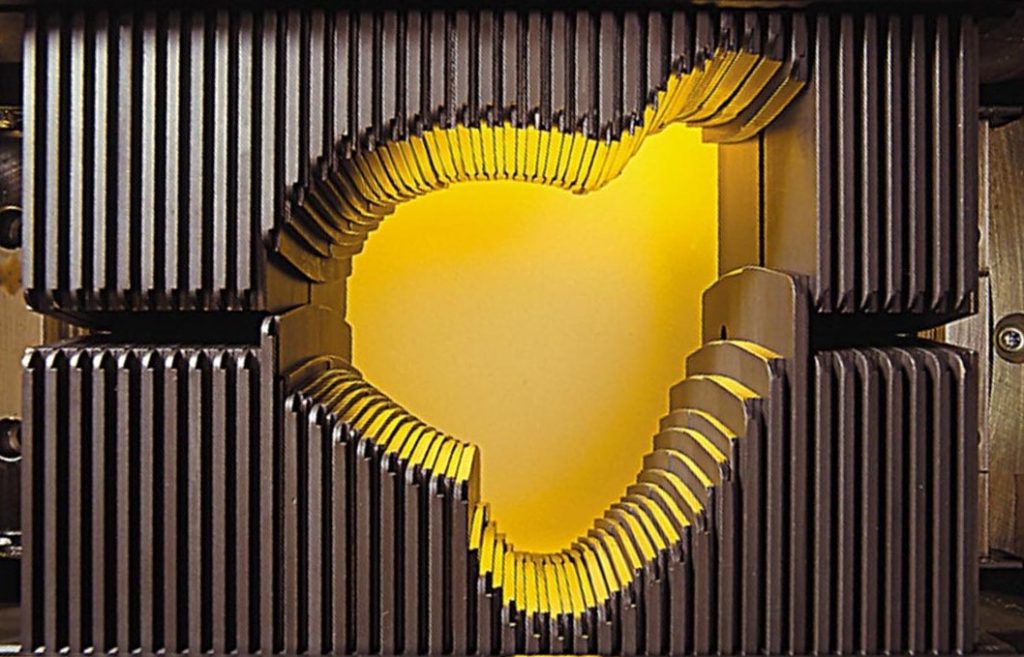
One treatment that may be employed is Intensity Modulated Radiation Therapy (IMRT). In this treatment, you are secured to a bed and a linear accelerator fires beams of radiation at the cancer cells from various angles. The beams are modulated by leaves that block parts of the beam, and the aim is to concentrate the beams on all of the cancer cells to fully irradiate it. This set of leaves is called a multi-leaf collimator.
IMRT machines have improved a lot over the past two decades and more complex treatments are possible. This allows more people to survive cancer with a low risk of the cancer returning.
This is great news, but complex treatment requires careful planning and traditionally this has been done by a skilled practitioner who often has years of experience. Ideally, much of the planning should be optimized automatically by computers (with guidance from practitioners) and this is what this blog series will explore.
The planning process is split into three phases, click each part to find out about the mathematical challenges to each part: