Aims: To assess the feasibility and effectiveness of a supported self-management package for relatives of people with recent-onset psychosis.
Method: A randomised controlled trial (n = 103) comparing treatment as usual (TAU) in early intervention services with TAU plus the Relatives' Education And Coping Toolkit (REACT) intervention (trial identifier: ISRCTN69299093).
Results: Compared with TAU only, those receiving the additional REACT intervention showed reduced distress and increased perceived support and perceived ability to cope at 6-month follow-up.
Conclusions: The toolkit is a feasible and potentially effective intervention to improve outcomes for relatives. A larger trial is needed to reliably assess the clinical and cost-effectiveness of REACT, and its impact on longer-term outcomes
Relatives of people with psychosis, including relatives who have used the previous version of the intervention influenced the content and current format of REACT website. Based on their feedback, we made the toolkit more suitable for a broader range of relatives, including those outside Early Intervention Services and for relatives supporting people with Bipolar Disorder. In addition, we made REACT more interactive and available online directly to relatives, and ensured that it was supported by Expert Relatives (someone with lived experience of supporting a person with mental health problems) rather than by NHS staff.
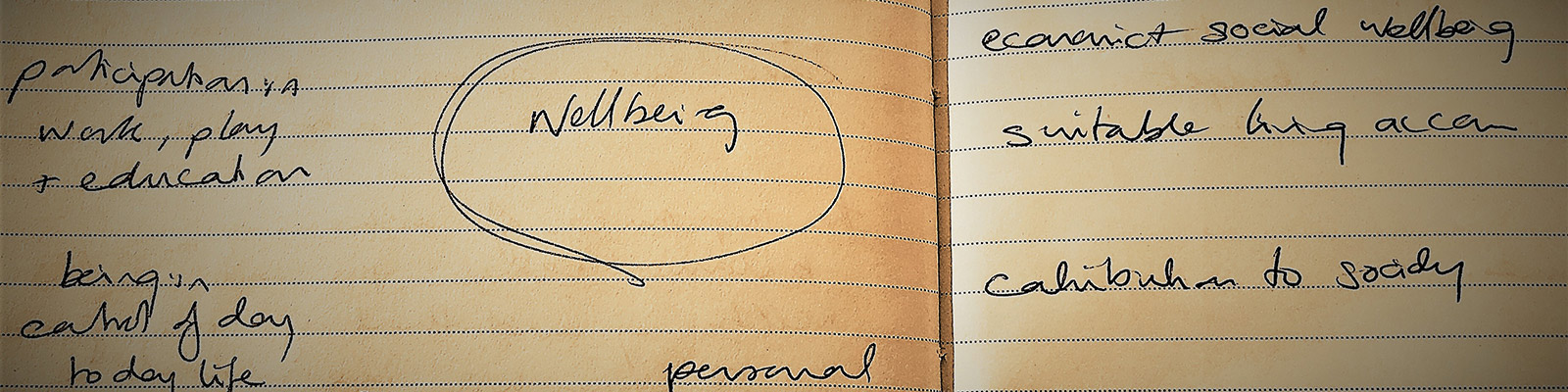
The results of the first trial showed that REACT is potentially effective to reduce distress in relatives and improve abilities to cope and support for relatives. However, the first trial included a small group of people, who received the toolkit from their Early Intervention Team. Therefore, the research team designed a larger scale research project to test whether REACT is effective in reducing distress in relatives and the cost for the NHS to support relatives, when it is delivered online and accessible for any relatives, who lived in the UK (not only the relatives, who received care from their NHS early intervention team). In this larger trial, relatives registered and used the REACT toolkit online. Half of them received the new interactive REACT toolkit, supported by Expert Relatives, and the resource directory (full range of support currently available to relatives of people with psychosis or bipolar disorder via national mental health organisations), while the other half received the Resource Directory only. Both groups continued to receive treatment as usual from their care providers. The protocol of how this trial was conducted has already been published and available below. The results of the trial will be available in Spring 2019 on this website. [Date may be changed]
View full-text of the article